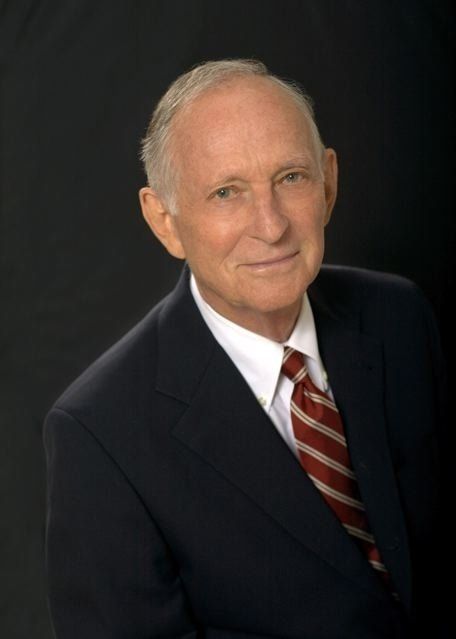
ROBERT C. KNAPP, MD, D.Sc (Honorary)
Board Member and Chairman of the Medical Advisory Board
William Baker Professor of Gynecology (Emeritus), Harvard Medical School
Visiting Scholar, Weill Medical College of Cornell University
Former Director of Gynecology, Brigham & Women’s Hospital
Former Director of Gynecology Dana Farber Cancer Center
To learn more about ovarian cancer, click HERE